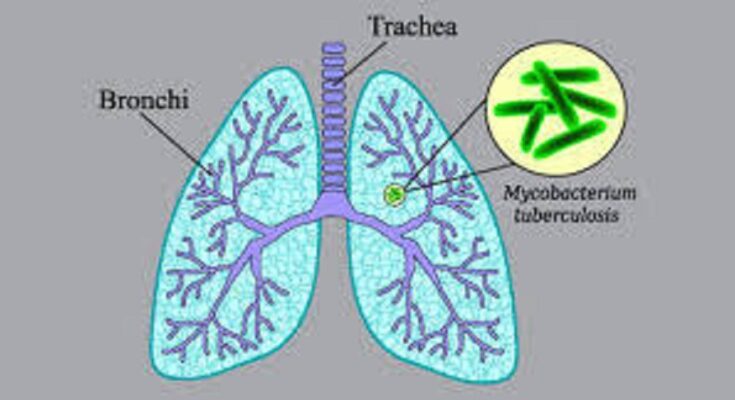
In our ongoing battle against infectious diseases, healthcare professionals consistently encounter formidable adversaries, Tuberculosis (TB) being one of them. Nonetheless, there is arguably no better opportunity to combat this disease than now, considering the current advancements in tuberculosis treatment. This article delves into the current landscape of TPT design, with particular emphasis on the National Guidelines for Tuberculosis Preventive Treatment (PM-TPT). These guidelines represent a breakthrough in the fight against TB as they provide detailed information about treatment regimens, dosages, and approaches to managing adverse reactions.
The Significance of Tuberculosis Preventive Treatment (TPT)
Tuberculosis Preventive Treatment (TPT) is a critical component in our strategy to eradicate the scourge of Tuberculosis. The rationale behind TPT is straightforward yet compelling. By diagnosing and initiating treatment for patients at high risk of developing active TB, there is an increased potential for controlling new TB cases, thus reducing its transmission and societal impact. Moreover, the National Guidelines on Tuberculosis Preventive Treatment offer comprehensive recommendations for the programmatic management of TPT. By adhering to these guidelines, beneficiaries receive essential, timely, and high-quality treatment, ensuring the safeguarding of their personal and social health, which is a paramount concern.
Identifying High-Risk Groups
This includes people in the same family with TB patients, positive TB patients, healthcare workers, and those with other illnesses such as diabetes. This way, we can address the preventive measures to the identified high-risk groups and individuals.
Screening and Diagnosis
Ensuring early and accurate diagnosis of TB is crucial for providing suitable treatment for the disease. Moreover, the guidelines delineate various approaches for implementing recommendations aimed at screening individuals at risk of TB, employing methods such as TST and IGRAs. These tests play a significant role in identifying individuals with latent TB infection (LTBI), who are the main target of TB preventive therapy (TPT).
Treatment Protocols for Tuberculosis Preventive Treatment
Since the treatment protocols presented in guidelines should be feasible, it is not surprising that they also aim at being effective. So It includes guidelines for the use of isoniazid, rifapentine, and other TB drugs, supplemented with pyridoxine (vitamin B6) to mitigate the neuropsychiatric side effects of isoniazid. Ensuring strict adherence to the antibiotic regimen within a specified timeframe is crucial for TB preventive therapy (TPT).The guidelines offer instructions on how to keep track of patients’ progress and the necessary interventions that need to be provided to the patients during the process of the treatment, including follow-up appointments, counseling, as well as other supportive means, such as utilizing technological tools for tracking patient’s progress.
Detailed Treatment Regimens and Dosages For Tuberculosis Preventive Treatment
These guideline outline different treatment care pathways for different patient populations with different needs. Here are some key regimens: Here are some key regimens:
1.Isoniazid Preventive Therapy (IPT)
Dosage
Isoniazid 300 daily for adults; 10mg / kg / daily for children with a maximum of 300mge.
Duration
Ideally, it takes between 6 to 9 months of evaluation time before an investment be ranked suitable for investing in.
Pyridoxine
25 mg daily to prevent neuropathy well: Since it is a well-known fact that neuropathy is one of the common side effects of the drug, taking 25 mg daily should prevent that from happening.
2.Rifapentine and Isoniazid (3HP)
Dosage
Rifapentine 900 mg/week and isoniazid 900 mg/week for adult patients.
Duration
3 months.
Pyridoxine
Rare at dose of 25 mg weekly with isoniazid.
3.Rifampicin
Dosage
Depending on the patient, the dosage is Rifampicin 600 mg daily for adults or 10-20 mg/kg for children.
Duration
4 months.
Pyridoxine
Only considered for high-risk patients as it is not typically necessary.
These regimens rely on various factors, encompassing the patient’s age, HIV status, and whether the patient is taking other medications that may interact with the SSRI. Shorter schedules like 3HP are preferred due to their enhanced compliance compared to extended regimens, as well as the minimal side effects observed.
Managing Adverse Effects of Tuberculosis Preventive Treatment
Toxic effects pose a major challenge to the treatment of TB, so we must watch them keenly to protect patients and maintain compliance. Here are the common adverse effects and management strategies. Here are the common adverse effects and management strategies:
1.Hepatotoxicity
Symptoms
Yeast infections, abdominal pain, jaundice, elevated liver enzymes, fatigue.
Management
Regularly conduct liver function tests; should hepatotoxicity be detected, contemplate adjusting the drug and its dosage accordingly. Moreover, in instances where hepatotoxicity is suspected, it might be prudent to substitute the hepatotoxic drug with a similar non-hepatotoxic alternative.
2.Peripheral Neuropathy
Symptoms
Some possible symptoms could be, sensations of prickling, numbness and weakness in the extremities.
Management
Supplementary prescriptions of pyridoxine (vitamin B6) if severe, consider modification of treatment plan.
3.Gastrointestinal Disturbances
Symptoms
Proper caused by nausea vomiting and /or abdominal pain.
Management
Give medication with food; use antiemetics sparingly for the patient.
4.Hypersensitivity Reactions
Symptoms
This one has hasty movements, nausea, fever, and joint pains.
Management
Patients require cessation of the offending drug and treatment of these symptoms may involve the use of antihistamines and corticosteroids drugs respectively.
Advancements in Tuberculosis Preventive Treatment
Several advancements in TPT are poised to revolutionize our approach, as highlighted by the guidelines.
Shorter Treatment Regimens
The traditional treatment dosage regimens for TB have also been long, with most extending to six to nine months. However, some recent studies have shown that other brief regimens like three months isoniazid-rifapentine, 3HP regimen is equally effective. These shorter regimens also decreases the likelihood of patients not following the prescribed treatment and also the side effects.
New Diagnostic Tools
Accomplishments in diagnostic techniques including the GeneXpert MTB/RIF have expanded capability to diagnose TB a lot quicker and precise. This test can diagnose TB and Rif resistant TB in significantly less than 120 minutes which will help the doctors to start right treatment immediately.
Digital Health Technologies
As digital technologies continue to advance, they are increasingly utilized in tuberculosis care. These technologies, such as smart applications and electronic patient records, play a pivotal role in tackling compliance issues, guaranteeing the timely administration of medication, and enabling consultations through electronic platforms. This not only enhances patient engagement but also has demonstrated efficacy in improving outcomes in numerous instances.
Implementation of the Guidelines For Tuberculosis Preventive Treatment
Education, training, and support for practitioners and healthcare organizations together with awareness raising for consumers and the public are the cornerstones for effective uptake of these guidelines. Here are some strategies to ensure effective implementation. Here are some strategies to ensure effective implementation:
Training and Capacity Building
Unfortunately, healthcare professionals particularly those in the rural health facilities require to have adequate knowledge in the current recommended treatment guidelines in managing TB patients, as well as knowledge of modern diagnostic techniques for the disease. Recurrent training programs and workshops within the medical community can effect updates in skills, competency, and knowledge regarding TB control.
Community Engagement For Tuberculosis Preventive Treatment
Community participation is paramount when it comes to making awareness of the disease as well as the promotion of preventive treatment. The involvement of the community health workers may include increasing awareness among the populace and both screening and monitoring such individuals who pose a high risk, as well as helping patients through their treatment journey.
Policy Support
It is important that there is a high level of support attributed to the governments and the health authorities in order to ensure that TPT programs are effective. This encompasses: TB financing such as donations for TB initiatives; TB R&D funding for new diagnosis, treatment, and prevention tools; and TB-friendly polices including funding for programs and systems.
Monitoring and Evaluation
Moreover, conducting cross-sectional checks and balances is recommended to evaluate the effectiveness of TPT programs. This process involves monitoring treatment outcomes, compliance levels, and the prevalence of TB within society. Through analyzing this data, we can identify areas necessitating adjustments or assess whether programs are successfully achieving their objectives.
Conclusion
Today, tuberculosis remains a prevalent disease, and we still have a long way to go before completely eliminating TB. However, advanced tuberculosis medications and the enactment of extensive guidelines make reaching that goal of TB elimination easier and more possible. Thus, it falls on healthcare professionals, such as myself, to contribute to this effort. By engaging in such activities, we stay abreast of the latest guidelines and recommendations for managing the disease. Additionally, we actively raise awareness among the public and ensure that our policies governing TB are robust, thus promoting the well-being of individuals affected by TB.
Furthermore, the National Guidelines for Tuberculosis Preventive Treatment offer clear and specific instructions for managing TB. Therefore, we must implement and perform these guidelines to the highest level. Consequently, we can make a difference toward eradicating TB and achieving the vision of a TB-free world. Thus, now is the time for us to welcome these changes with enthusiasm and commitment, as we know our efforts can save lives and transform communities.